- Home
- Distal Femoral Osteotomy
Distal Femoral Osteotomy
Distal Femoral Osteotomy
There are a number of different indications for a distal femoral osteotomy. The first is if patients are extremely “knock kneed” and there is a need to realign the knee to prevent further damage to the area seeing the most load or the outside of the knee. The second is in patients who have arthritis on the outside of the knee and are too young for a standard partial knee replacement. Also, partial knee replacements of the outside of the knee do not last as long versus inside partial replacement so there is even more reason to consider distal femoral osteotomy compared to knee replacement. Generally, these patients are younger than 55 years old. If patients have “knock kneed” knees and arthritis this can be a very effective surgery and delay the need for a knee replacement. This realignment moves the force on the arthritis part of the knee to the normal part. The final patient type is very young patients who need cartilage, ligament or meniscus transplant procedures with alignment issues. This surgery is very successful in these cases and can dramatically improve success of these procedures if done in conjunction. For the meniscus and cartilage transplant patients “realigning” the knee can increase the healing of the transplant and improve survival
Description:
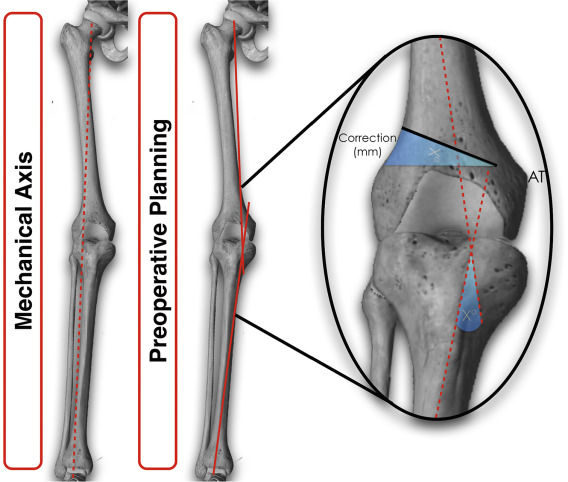
A distal femoral involves a surgical cut of the bone at bottom of the femur. Generally, a hinge of 8-15 mm is made to improve the alignment and offset potential issues of the knee. Usually bone graft, plates, and screws are used to hold open the distal femoral osteotomy. Some distal femoral osteotomies involve taking out bone where you let the leg compress on itself, this is called a closing wedge distal femoral osteotomy. Most osteotomies done are opening wedge as previously described.
How do you determine if you need an osteotomy?
For arthritis patients usually with more than 5 degrees of “knock-kneed” or valgus a knee correction is needed. For cartilage patients the cut off is slightly lower at 3-4 degrees of valgus. Once this is indicated, Dr. Garcia will discuss when this portion of the surgery will occur, or if a separate surgery is needed.
BOOK AN APPOINTMENT
“KNEEO Technique” For Knee Replacements
OPERATION
The operation is performed in a sterile operating theatre, with the patient under a general anesthetic.
The operation is performed as an open procedure with the incision on either the inside or outside of the distal thigh and knee, depending upon the specific surgery being performed .
The thigh bone (femur) is exposed and then either a wedge of bone resected, or a wedge of bone inserted. X-rays are taken throughout the procedure to ensure that the mechanical axis is corrected appropriately. Following this the bone cut is stabilised with a metal plate and screws, that holds the bones in place until the bone has healed.
The knee is placed in a range of motion brace until the bone has healed, and this is at least 2 months.
Patients will spend at least one night in hospital and will be on antibiotics for at last 6 days, and a blood thinner. Patients are only allowed to partial weight bear for 2 months.
Potential complications
1. Infection
There is a 1% risk of superficial wound infection, which may respond to oral antibiotics. There is a lower risk of deep infection but this usually requires a return to theatre to wash the wound out as well as intravenous antibiotics.
2. Delayed union or non-union
Sometimes the osteotomy can take longer than 2 months to heal, and on rare occasions it does not heal. The latter may require a return to the operating theatre to either add further bone graft and / or redo the operation.
3. Thrombosis or DVT
The surgery and period in the brace increases the risk of developing and thrombosis or DVT. For this reason the patient is placed on a blood thinner for at least 10 days to reduce the risk of this occurring.
4. Nerve or vessel injury
Because the surgery involves cutting through the femur, there is a risk fo damage to the nerves and vessels lying behind the bone. This is a serious potential complication and Dr. Porter ensures that these structures are protected before he cuts through the bone.
5. Recurrent pain and need for a knee replacement
Although most patients experience significant relief of their pain, the duration of relief is hard to predict. The patient still has to protect the knee and exercise the measures shown to slow the progress of the wear and tear in the knee. In some patients the pain does come back earlier than expected and the only solution may be conversion to a knee replacement.


