- Home
- Management of Multiligament knee Injuries
Management of Multiligament knee Injuries
Management of Multiligament knee Injuries
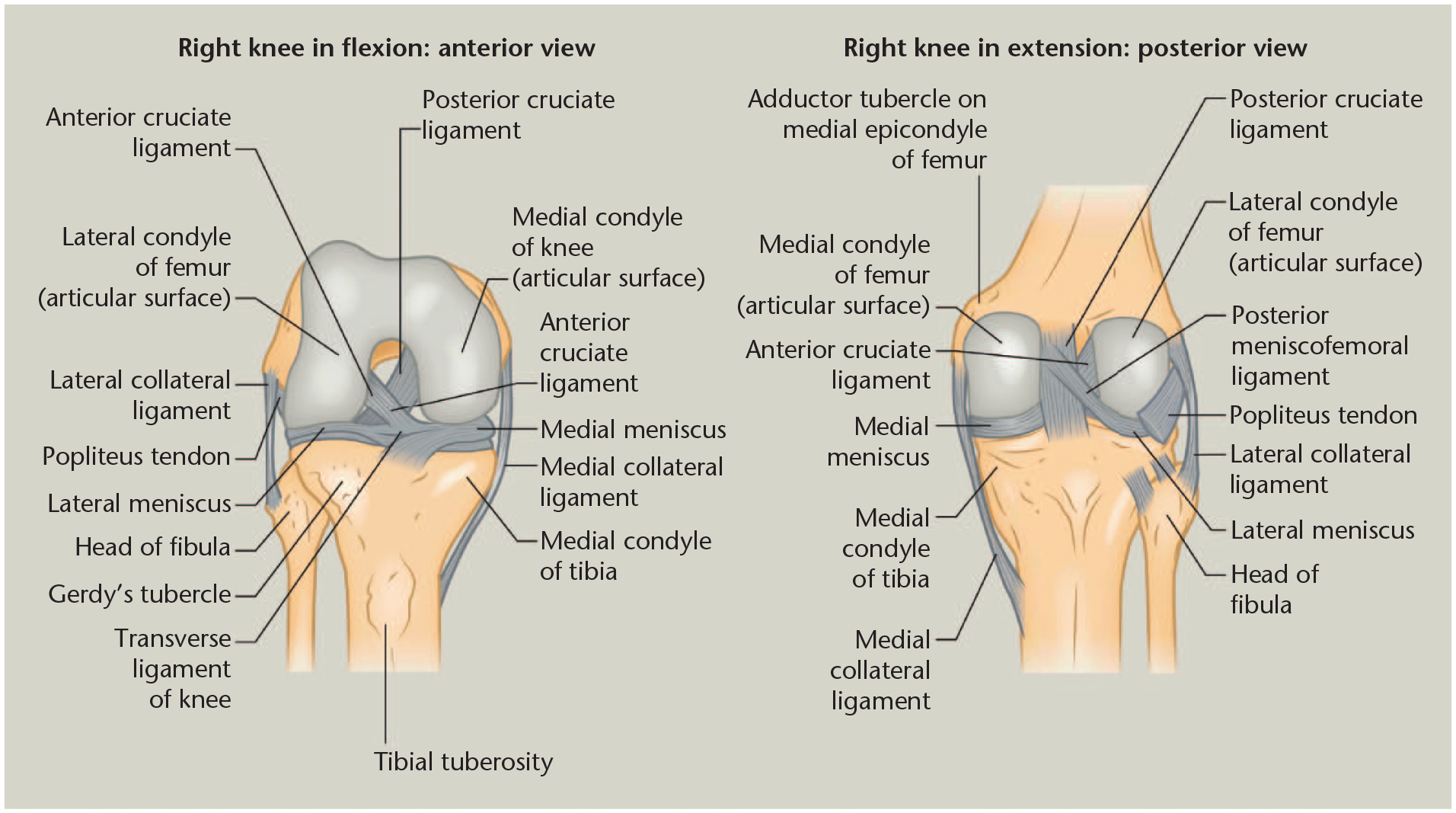
Multi-ligamentous knee injury (MLKI) is a rare but serious injury of the knee and is defined as involving at least two of the four main knee ligaments: the anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), posteromedial corner (PMC) including the medial collateral ligament (MCL), and posterolateral corner (PLC) including the lateral collateral ligament (LCL). Mechanisms of injury often involve acute knee dislocation secondary to high velocity trauma (i.e., motor vehicle accident) but can also be secondary to low -velocity injury that arise from sporting events (1). Early care management involves critical assessment of soft tissue integrity and patient neurovascular status as both peroneal nerve and popliteal artery are at risk. Early knee reduction is important as to best relieve tension stress on neurovascular structures.
Conservative management
The indications for non-operative management are few, as most patients will require surgical management barring comorbidities that preclude surgery. Current indications are patients with low-functional demand, severe polytrauma, significant head injury, and extensive soft tissue damage above the knee. Nonetheless, outcomes can be optimized for patients undergoing conservative management, although this is not expected to mirror results obtained from surgery. Important points to consider are an expeditious closed reduction after knee dislocation with care taken to avoid the popliteal fossa as to not compromise arterial flow. After reduction, the knee should be immobilized in 15 to 20 degrees of flexion with a subsequent arteriogram conducted to assess vascular compromise. It is important to note that the use of doppler ultrasound has been controversial due to occult intimal thrombosis in the presence of normal pulses. Magnetic resonance imaging can be conducted one week after initial injury to assess for ligamentous damage. Rehabilitation should entail range of motion exercises that emphasizes extension. Isometric exercises should be conducted to strengthen quadriceps and hamstring muscles.
BOOK AN APPOINTMENT
“KNEEO Technique” For Knee Replacements
Developing evidence-based guidelines
The most confident conclusion that can be made after careful analysis of the literature is that optimal operative strategy is most likely closely dependent on injury characteristics. It appears that acute repair has utility in treating avulsion fractures. Acute repair may also be a suitable strategy for injuries to the corners and collateral ligaments, however this not certain considering higher rates of failure of repair vs. reconstruction found for both the PLC and PMC in comparative studies . Although it appears that reconstruction may be optimal for cruciate injury, and is certainly preferred in practice, no high-level evidence exists to conclude this with certainty. It should also be noted that the literature may underestimate the efficacy of modern reconstructive techniques as they have rapidly evolved in recent years. Comparisons of repair vs reconstruction are in general complicated by this evolution of reconstructive techniques as well as the variety of different techniques that are now available.
Optimal operative timing also likely depends on injury characteristics however how so is not clear. There appears to be more evidence supporting early or staged intervention. This may reflect the fact that the surgeon has more flexibility in the techniques he can use if an acute intervention is incorporated. In most evaluations of early or staged interventions, repair was utilized in the acute phase, which is suggestive of its utility, and circles back to the debate of which structures if any are more amenable to repair vs. reconstruction. There are conflicting reports however with others suggest a superiority of delayed surgery. The benefit of delayed reconstruction may furthermore be underestimated due to selection bias, since surgery is more often delayed in patients with more serious injuries as they cannot tolerate acute surgery.
The most notable characteristic of the body of evidence concerning operative management of MLKI is a marked lack of high-quality data. The literature primarily consists of retrospective case series with small sample sizes. Very few prospective and/or comparative studies of different surgical treatments for MLKI have been published. Comparative studies were also characterized by small sample size. Moreover, these were not randomized and most involved a population that was highly heterogeneous in both injury and patient characteristics, creating high potential for selection bias. Both within and across all studies there is a high degree of variability with respect to patient and injury characteristics, operative techniques, rehabilitation protocol, and evaluation of outcomes, which limits the ability to systematically review and draw conclusions from them.


