- Home
- Osteochondral Autograft transfer
Osteochondral Autograft transfer
Osteochondral Autograft Transfer
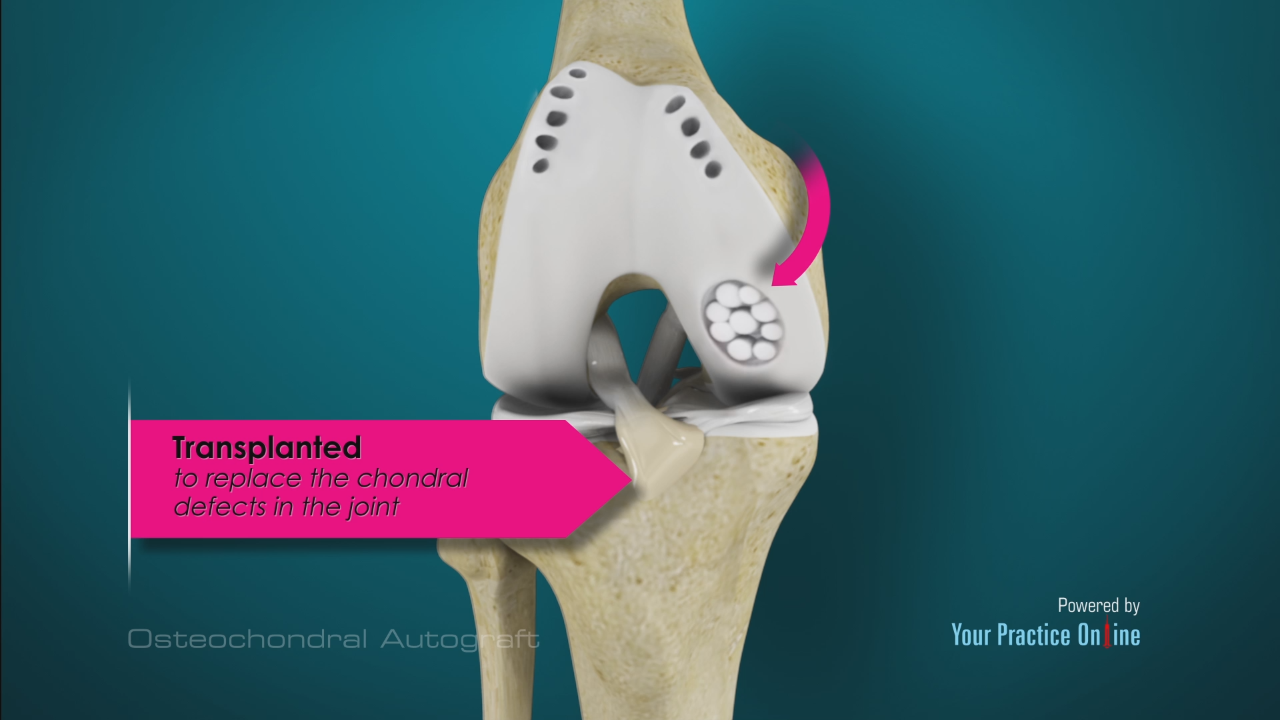
This technique involves taking small amounts of bone and cartilage from low-weight-bearing parts of the femur (thigh bone) within the knee and transferring them to the higher-weight-bearing area of injury. This grafting can be performed through arthroscopy, open technique or mini-open technique through a small incision. Often, arthroscopy is used for diagnosis, and then a mini-open approach is used to complete the procedure. The size and shape of the defect is determined, and it is prepared using the appropriate equipment. The area of the femur from which the grafting material will be taken will be selected based on the size and shape of the injured area. A harvesting chisel is used to remove the tissue, which is then inserted into the prepared area.
One of the main advantages of this procedure is that it results in mature, healthy cartilage at the defect site. In addition, it can successfully be used to correct bone loss or an abnormality. However, it can negatively affect the area from which material is harvested, and the amount of material available can be limited. Therefore, this approach is best for correcting small defects.
Rehabilitation
Post-operative rehabilitation consists of toe-touch weight-bearing for 4 to 8 weeks, depending on the extent of grafting performed. Early, progressive motion is encouraged with special equipment, and a return to athletic activity is delayed for 4 to 6 months.
Outcome
Most studies report good-to-excellent results in up to 90 percent of patients treated for specific types of defects. Smaller defects tend to do better than larger defects.
BOOK AN APPOINTMENT
“KNEEO Technique” For Knee Replacements
Abstract
Osteochondral autograft transplant (mosaicplasty) is a cartilage repair procedure for patients with knee articular cartilage lesions of a substantial size (>3 cm2). Patient selection is key to a successful result; patients with established osteoarthritis or systematic disorders such as rheumatoid arthritis should not undergo surgery. An exercise program involving neuromuscular training for a minimum of 3 months should be attempted before proceeding to osteochondral autograft transplant. The procedure can, in many cases, be performed arthroscopically. Patients should, however, provide consent for a mini-arthrotomy as this might be needed to achieve optimal access for graft harvesting and insertion. The procedure, in general, consists of 4 major steps.
(1) At the initial arthroscopic examination, the size and localization of the defect are assessed after a proper debridement has been performed. The number and size of autografts needed can thereafter be assessed.
(2) Graft harvesting is then performed from the periphery of the non-weight-bearing trochlea.
(3) To prepare for graft insertion at the recipient site, a drill guide is inserted perpendicular to the joint surface in the defect to allow graft sockets to be reamed.
(4) Grafts should be spaced approximately 3 mm apart to avoid confluence of tunnels and weakening of condyles. The orientation and depth of insertion of the grafts are key to mimic the native curvature of the affected joint surface.
After an initial phase of non-weight-bearing focusing on range of motion, a gradual increase in neuromuscular exercises is recommended. Patients are typically advised to delay their return to sports until 6 months at the earliest. Results after mosaicplasty have shown that the procedure improves subjective outcomes, compared with baseline function, for up to 10 years after surgery. The additional effect over traditional microfracture treatment is, however, reduced over time. A study evaluating early factors affecting outcomes after cartilage repair procedures (including mosaicplasty) found that a series of factors, such as the time from the onset of symptoms to surgery, number and size of lesions, location and quality of surrounding cartilage, as well as concomitant meniscal injuries, were important.


